What Are The Health Risks?
"Obesity contributes to the risk of dying not only from heart disease and diabetes but from cancer."
(New Eng J Medicine, April 2003)
"Obesity will soon overtake smoking as the primary cause of preventable death if current trends continue."
(American Medical Association, January 2003)
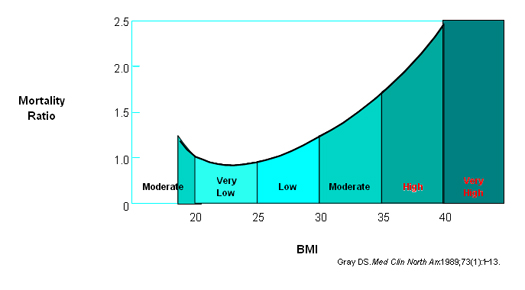
Premature Death
Your annual risk of dying from obesity-related causes doubles at a BMI of 35, and rises considerably as your BMI increases above this level.
Associated Health Risks
There are many medical conditions that are caused, or worsened, by obesity. These include:
- High blood pressure
- Type 2 diabetes
- Heart disease, including coronary artery disease and heart attacks
- Sleep apnoea and snoring
- Asthma
- Arthritis of the hips, knees and back
- High cholesterol and lipids
- Gallstones
- Acid reflux or heartburn
- Cancer risk: breast, ovaries, cervix, uterus, colon, gallbladder and prostate
- Menstrual irregularities and infertility
- Incontinence
- Hirsutism
- Strokes
- Depression
- Venous stasis ulcers
- Intertrigo and other skin infections
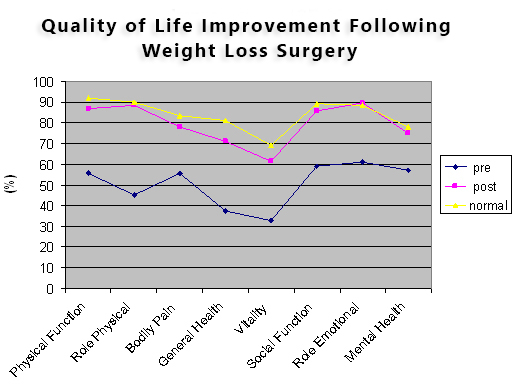
Psychological Impact and Social Wellness
Obese people may experience psychological and/or social problems which can often lead to social isolation. They may experience:
- Low self esteem
- Low self confidence
- Poor self image
- Depression
- Discrimination at home and in the workplace
- Sexual limitations
They may also experience physical limitations due to their weight. Normal daily tasks might be difficult to perform as they tire quickly or just run out of breath while clothes shopping, getting in and out of cars and personal hygiene may be difficult.